Dry Eye Corner Part 2

Measuring the impact of DED on patients’ daily lives is a critical aspect of disease characterisation
Dry eye disease (DED) is one of the most prevalent ocular surface conditions in the world.
It has been reported to occur globally within the range of approximately 4.4 per cent to as much as 50 per cent in the middle-aged and older population1-8. With the changes in lifestyle and increased use of tablets and phone screens, we are now finding DED in younger people too.
Measurement of the impact of DED on patients’ daily lives is now recognised as a critical aspect of the disease characterisation. Understanding how DED affects everyday activities helps us, clinicians, better evaluate the severity and progression of the condition, as well as the effectiveness of various treatment approaches.
Social media listening study
A paper published in 20199 was the first study to use social media listening (SML) to understand patients’ experiences of living with DED. SML is the strategic process of monitoring and analysing online conversations (utilising mentions, keywords, trends, sentiment, etc) about a subject.
After filtering for the most relevant online conversations to this study, 1,192 posts were analysed; 99 per cent were made directly by patients and most came from the USA (77 per cent) or the UK (21 per cent).
Only 130 posts gave any clue as to gender and, of these, 68 per cent were female and 32 per cent were male. Where age could be discerned, 39 per cent were 21 to 30 years old, 12 per cent were aged 31 to 40, and 22 per cent were aged between 41 and 50 years.
Key themes discussed online
The key themes discussed in the online conversations were, in decreasing order: management, symptoms, causes, diagnosis, and associated comorbidities.
Eye dryness, pain and blurry vision were the most common symptoms mentioned, whilst the most popular cause, with 40 per cent of the posts, was underlying medical conditions, such as Sjögren’s syndrome, blepharitis, vitamin D deficiency and autoimmune conditions.
Perhaps unsurprisingly, 24 per cent of posts mentioned eye surgery as a cause, including cataract and various forms of refractive surgery. Side-effects to medication were the subject of 15 per cent of posts, which included contraceptives, antihistamines, blood pressure medication, isotretinoin and cancer medication.
Eye disease, autoimmune conditions, thyroid disorders and diabetes were the most common comorbidities. The Schirmer test and tear film break-up time were the most common of many diagnostic methods discussed.
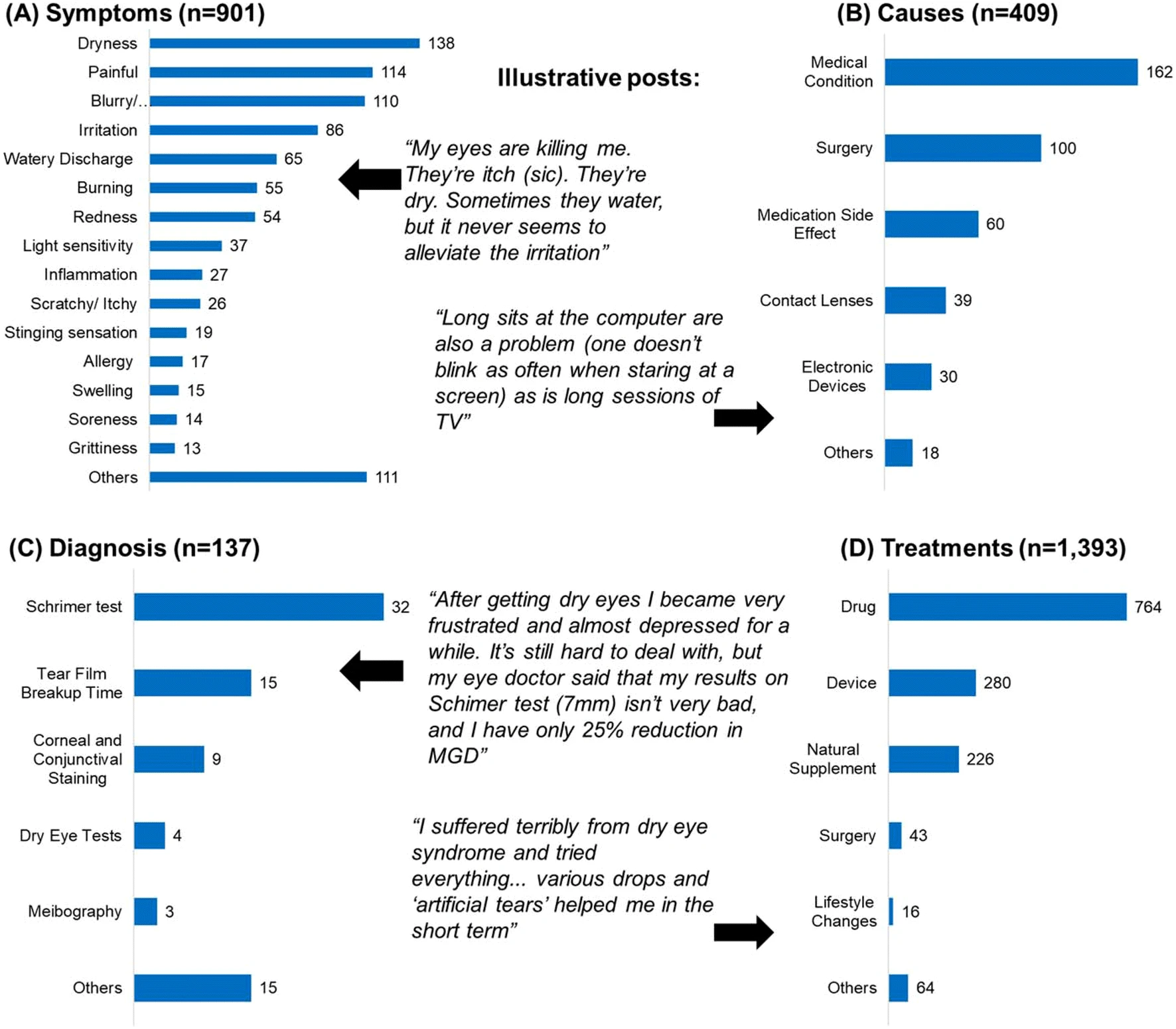
Major themes of discussion on social media by the number of mentions in the posts
DED impact of quality of life
The profound impact of DED on the patient’s quality of life (QoL) was mentioned in 224 posts, often restricting the poster’s ability to perform everyday tasks. Many individuals with DED reported significant challenges in their daily routines, including difficulties with commuting, driving and using electronic devices.
These limitations extended beyond practical inconveniences, with the condition also exerting a considerable impact on psychological well-being. This was evident from patients’ own accounts.
Among the documented quotes regarding QoL, nearly one quarter (51 out of 224) specifically referred to difficulties encountered in the workplace. Notably, of these 51 workplace-related mentions, 48 described negative experiences, underlining the substantial effect DED can have on professional life.
Everyday activities such as driving, reading and wearing contact lenses were among those most frequently associated with negative experiences. The overlap between these activities and the reported reduction in QoL highlights the close connection between the clinical symptoms of DED and the daily experiences of those affected.
These were the most commonly mentioned aspects of the negative impact of DED on QoL:
• Workplace difficulties: Can’t work on the computer, can’t keep up with work, can’t focus on work, stopped working, can’t work full time, trouble finding job and retired early
• Electronic device usage: Eye strain, unable to use, difficulty in reading and blurry vision
• Reading difficulties: Can’t read, eyes burn while reading, difficulty in reading and blur while reading
• Driving: Difficulty in driving, can’t see when driving, stopped driving, night driving is difficult and trouble concentrating
Also mentioned were: having to stop wearing contact lenses; can no longer watch a movie or TV; and being socially awkward or even missing social events.
The paper concludes that: “DED imposes a significant burden of impaired QoL in patients that spans multiple aspects of daily life. This appears to manifest itself in terms of both a requirement for more efficacious treatment options and also improvements in the education, diagnosis and management of the disease”.
After reading this paper, the author’s opinion is that we, as eyecare professionals, need to ensure that our knowledge and diagnosis of the different types of DED is up-to-date. It is also important to fully understand what treatments would be most efficacious in each dry eye patient we encounter.
References
1. Bjerrum KB. Keratoconjunctivitis sicca and primary Sjogren’s syndrome in a Danish population aged 30-60 years. Acta. Ophthalmol. Scand. 1997;75:281-6.
2. Schein OD, Munoz B, Tielsch JM, Bandeen-Roche K, West S. Prevalence of dry eye among the elderly. Am. J. Ophthalmol. 1997;124:723-8.
3. McCarty CA, Bansal AK, Livingston PM, Stanislavsky YL, Taylor HR. The epidemiology of dry eye in Melbourne, Australia. Ophthalmology 1998;105:1114-9.
4. Shimmura S, Shimazaki J, Tsubota K. Results of a population-based questionnaire on the symptoms and lifestyles associated with dry eye. Cornea 1999;18:408-11.
5. Moss SE, Klein R, Klein BE. Prevalence of and risk factors for dry eye syndrome. Arch. Ophthalmol. 2000;118:1264-8.
6. Yazdani C, McLaughlin T, Smeeding JE, Walt J. Prevalence of treated dry eye disease in a managed care population. Clin. Ther. 2001;23:1672-82.
7. Schaumberg DA, Sullivan DA, Buring JE, Dana MR. Prevalence of dry eye syndrome among US women. Am. J. Ophthalmol. 2003;136:318-26.
8. Guo B, Lu P, Chen X, Zhang W, Chen R. Prevalence of dry eye disease in Mongolians at high altitude in China: the Henan eye study. Ophthalmic. Epidemiol. 2010;17:234-41.
9. Nigel Cook, Anmol Mullins, Raju Gautam, Sharath Medi, Clementine Prince, Nishith Tyagi, Jyothi Kommineni. Evaluating patient experiences in dry eye disease through social media listening research. Ophthalmol. Ther. 2019;8:407-420.
Next month, Keith will share his experiences in setting up a dry eye clinic, and offer some guidance on what it takes to get started.
Keith Tempany FBDO CL FBCLA qualified in 1976 and worked in both independent and multiple practice before opening a fee-based contact lens only practice in 2002. He is a fellow and a past president of the British Contact Lens Association (BCLA) and oversaw the development and launch of its Myopia Management Certificate. Keith is the store director of Leightons & Tempany Opticians & Hearing Care in Poole, and works as an independent consultant. He is an experienced author, lecturer and facilitator of contact lens and dry eye education both nationally and internationally.