England
England
This page provides information on and links to England specific regulations, enhanced services and updates on national/ local activity.
Primary care coaching
Updates
Primary Care Support England
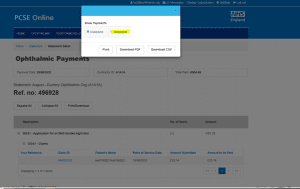
Printing your statement in full
The results of our Ophthalmic annual survey show that some practices are unable to see the entire statement when downloading it from PCSE Online.
The reason for this is that the collapsed view of the statement is being downloaded or printed.
To view your statement in full, simply select ‘Expanded‘ rather than ‘Collapsed‘ after you have clicked on the Print/Download option. This ensures all data will be included when you print or download your statement.
You can find more information about statements in any of the GOS user guides, available on the Ophthalmic Payments Resources web page.
Signatures not saved with draft GOS claim
We have been asked why Performer or Contractor signatures on saved draft GOS claims are not there when the claim is re-opened.
If any claim form is modified, for example, update an incorrect spelling of a patient’s name or a correction to a prescription, the signature is removed because the Performer and/Contractor will need to check and sign for the modifications.
The Performer and/or Contractor will need to sign the claim again prior to submission.
GOS claim submission window
We would like to also remind you of the validity period for GOS claims:
- GOS1, GOS5 and GOS6 – this is 3 months from date of sight test,
- GOS3 and GOS4 – this is 3 months from date glasses/contact lenses are supplied/collected
Please note: the 3 month period includes the submission of all claims. Please bear this in mind when submitting claims in PCSE Online or your PMS provider.
The 3 month window for submitting any outstanding paper GOS3 or GOS4 claims up to and including 31 December 2023, ended on 31 March. Any paper claims received after this date will be rejected.
Should you have have any GOS3 or GOS4 claims that were started prior to 1 January 2024, however are uncollected, these can be submitted on paper and the below 3 months window will not be applied. Please follow the uncollected process of making reasonable attempts to contact the patient. Guidance, provided by the professional bodies, on making accurate claims is available here should your practice require more information.
HC5 patient refund forms
From 1 April 2024 HC5 refunds are made by BACS.
In preparation for the implementation of ISFE2 in 2024, new HC5 claim forms are in circulation which allow patients to request a BACS refund for the cost of a sight test, glasses or contact lenses on low income grounds.
These HC5 forms are available for contractors to order in bulk and ICBs are expected to make refunds by BACS where a patient has requested this.
HC5 patient refund forms will continue to be submitted to the NHS Business Services Authority (NHSBSA) at the address stated in section 4 of the form, however from 1 April 2024 any HC5 forms that do not include the Patient’s bank details in Part 2 of the form will be rejected by NHSBSA.
Where bank details have not been captured, have been captured incorrectly or are incomplete, the HC5 form will be returned to the contractor for them to follow up with the Patient.
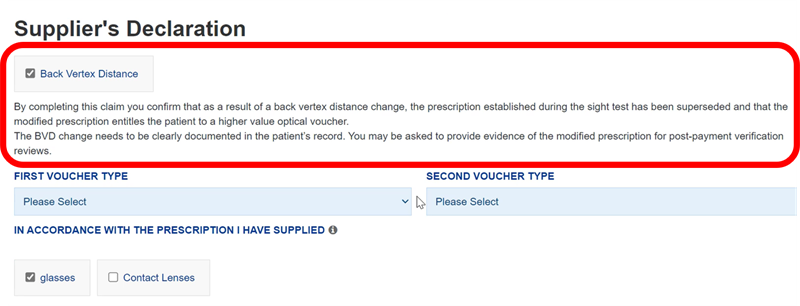
Adding supplements on PCSE Online for GOS3 and GOS4 claims
For GOS3 and GOS4 claims, PCSE Online does not automatically include supplements, even if these have been added to the prescription.
To ensure stores are paid correctly for the glasses/contact lenses supplied, we recommend the following:
- the prescription should include all required supplements
- all required supplements should be selected in the supplier declaration section
These two steps will ensure the supplements are included in the total claim.
This applies to both GOS3 and GOS4 claims. The supplier declaration claim is section 4 in a GOS 3 claim and section 5 on a GOS 4 claim.
For example, if the prescription includes a Prism/Tints supplement, the supplier declaration claim section does not automatically include these for the claim. The supplements will need to be selected, or the fee will not be paid.
In the screenshot below, there are no supplements included in the prescription, therefore they cannot be selected on the supplier declaration claim section, and will not be included in the total claim.
You can find more information, with screenshots, here.
Continuing professional development allowance
NHS England have confirmed that the payment for continuing professional development, undertaken between 1 January and 31 December 2023 by optometrist, will remain at £596. This relates to optometrists and ophthalmic medical practitioners without another medical appointment.
This payment was previously called continuing education and training (CET).
The claim window will open on 1 July 2024 and close on or before 31 October 2024. We will publish more information on the PCSE website in due course.
Managing the communications you receive
We send communications to our customers based on the roles they have on their PCSE Online accounts. This is to ensure that the content in our communications is appropriate for individuals within a practice.
For example, if we need to communicate a message about the continuing professional development (formerly CET) claims, we will send an email to PCSE Online users who have the ‘GOSPerformer’ and ‘ContractorSignatory’ roles required to create, sign and submit a continuing professional development claim.
If you receive a communication which you believe is not relevant to your current role, please speak to your User Administrator to remove any PCSE Online role(s) that you no longer require. PCSE will not remove roles from a user’s account and we will advise them to speak to their practice user administrator should we receive a request to do so.
Up to date user management will prevent users from continuing to receive emails sent specifically to your practice.
We now have a ‘Subscribe’ option for primary care colleagues, who do not have a PCSE Online account, to receive additional communications in areas of interest/relevance to them. You can find the link to subscribe on the PCSE website News page.
Read here.
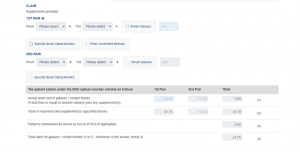
Changes in PCSE Online from January 2024
Uncollected glasses – GOS3 and GOS4 only. PCSE Online will allow for uncollected glasses to be processed electronically from 1 January 2024.
If a claim is started on PCSE Online before 1 January 2024 and accessed after 1 January, the new functionality will be visible.
A preview of the change in PCSE Online is below:
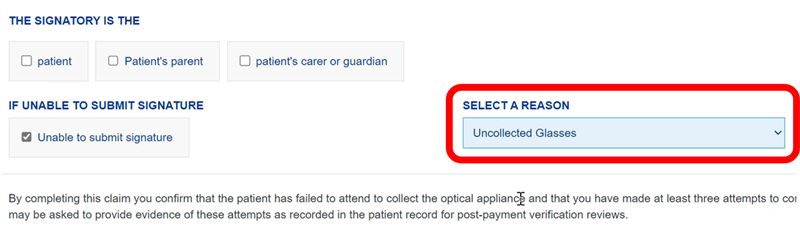
Back Vertex Distance (BVD) – GOS 3 only. PCSE Online will allow for claims for change in prescription flagged as BVD from 1 January 2024.
If a claim is started on PCSE Online before 1 January 2024 and accessed after 1 January, the new functionality will be visible.
A previous of the change in PCSE Online is shown below:
Please note, upon collection of glasses, where there has been a change in the voucher value as a result of the BVD claim, you must record this change in prescription on the patient’s clinical file.
Claim periods for sight tests – GOS1, GOS5 and GOS6 sight tests undertaken from 1 January 2024 will have a 3 month claim period. Any sight test undertaken prior to 1 January is still managed under the old regulations i.e. 6 month claim period.
You can find more information about all GOS related changes in the 11 October communication from NHS England.
12 October 2023
Read letter here.
14 June 2023
Read letter here.
Primary eye care has long been able to deliver a wide range of NHS care outside hospitals, including diagnosis, treatment, follow-up to surgery, and the co-management of long-term conditions.
Through NHS England’s National Eye Care Recovery and Transformation Programme, commissioners are being encouraged to take advantage of the full range of clinical expertise and infrastructure primary eye care has to offer, recognising it as the equivalent of general practice.
This is driven by the need to tackle outpatient waits, eliminate the risks of avoidable sight loss and address hospital capacity pressures which existed prior to Covid, and have increased significantly during the pandemic. The expansion of care outside hospital is also key to outpatient transformation and bringing the benefits of integrated care closer to home for an ageing population.
To help the NHS achieve this vital service transformation, the national optical bodies have worked with NHS England to develop an Optometry First model to be commissioned at scale utilising a consistent service specification.
Optometry First describes a comprehensive primary eye care service. It builds on the principles of CUES and reflects the vision of the College of Optometrists, Royal College of Ophthalmologists and wider optical representative bodies for a joint vision for safe and sustainable patient eye care services.
It will improve efficiency and accuracy of case-finding, extend the scope of care available within primary eye care and improve patient experience and opportunities for self-care. The model employs the core competencies of optometrists, dispensing opticians and their practice team, supported by higher qualified primary care practitioners and the multidisciplinary hospital ophthalmology team, where necessary, across a network of local optometric practices and the hospital eye service.
The service will ensure that primary care practitioners can offer first contact care through to resolution whilst also providing continuity of care for people with a long-term condition closer to home.
NHS England now wishes to test this model by working intensively with a small number of systems, as well as continuing to work more widely, with a view to strengthening the evidence base and demonstrating a route to scaling up across England. This is an approach supported by all optical bodies.
The willingness of primary eyecare to participate is a key criterion for ICS selection. Therefore, we are urging practices and their whole practice teams to demonstrate their willingness by getting involved if their area is selected to test this new model of care. In the first instance please contact your LOC for further information who will link directly with the ICS, LOCSU and other representative organisations.
If you would like to learn more about Optometry First, please contact your LOC, LOCSU or your representative body. You can also apply for an account on the FutureNHS Collaboration Platform and view the Optometry First Toolkit online.
| Afghan relocation and resettlement schemes – guidance for optometry practices
Individuals and families arriving into the UK under the Afghan Relocations and Assistance Policy (ARAP) scheme or Afghan citizens’ resettlement scheme (ACRS) will be entitled to free NHS care. People supported by UK Visas and Immigration (UKV&I) under section 95 are issued with HC2 certificates, usually within 2 weeks of their arrival. However, if the patient attends an optometry practice but has not yet received their HC2 certificate, the advice to the practice is as follows: · Do not refuse the eye care service, or see them as a private patient. · Complete the GOS form as standard, recording the bridging hotel as the patient’s address. · Tick ‘Universal credit’ as the eligibility criteria. · Tick the ‘Evidence not seen’ option. · Keep a note on the patient’s record that the eligibility category had been selected as per guidance from NHS England & NHS Improvement on submitting GOS claims for Afghan refugees. |
Read the England Health and Care Bill here.
Results from a CCEHC survey highlight the need to review commissioning and provision of low vision services to deliver more accessible and integrated care for patients in England.
The Clinical Council for Eye Health Commissioning (CCEHC) which represents the major clinical professions and sight loss charity organisations in the eye-care sector, has conducted a survey on the commissioning and provision of low vision assessment services in England.
The survey was conducted for five weeks from 5th April 2021 to gain an understanding of the impact of the pandemic on low vision assessment services between April 2020 – March 2021. The survey showed that prior to the pandemic, there was variation in the use of service specifications, protocols and thresholds for low vision assessment. Since the pandemic service provision has been challenging, with deployed clinical staff, patients and some practitioners shielding, and lower clinic numbers to maintain distancing. This has been associated with a significant fall in certifications of visual impairment during lockdown periods.
You can read the survey results here.
Based on these findings, the CCEHC makes the following recommendations, and calls for low vision services to be included in system recovery and transformation planning:
Manage low vision assessment backlogs by:
- risk assessment of patients waiting to prioritise those in greatest need.
- triage to interim support by another part of the system.
- aiming to clear backlogs within 6 months.
Review existing low vision service provision (demand and capacity), protocols and pathways to:
- scope potential for more integrated services
- incorporate remote consultations for prioritisation and follow-up as appropriate e.g., patient initiated follow up, access to advice and guidance, review to check managing with existing aids/ new requirements.
- ensure there is domiciliary provision for those that require it.
- ensure Eye Clinic Liaison Officers are core members of the low vision service team and link across primary, community, hospital and social care.
- include provision of information on digital assistive aids (e.g., digital magnifiers) and signposting to IT courses for those who are visually challenged.
Develop service specifications and quality standards for integrated low vision care as part of a whole systems approach to:
- ensure consistent access and availability of services.
- offer a choice (where possible or appropriate) making optimal use of primary, community, local authority and hospital services.
- provide processes for governance, audit, engagement, service improvement, and review of services provided.
- identify a dedicated (ring fenced) low vision budget that can be accessed system wide (primary, secondary and tertiary) to ensure a sustainable service.
Ms Parul Desai, CCEHC Chair commented, “Many providers have tried to ensure safe services and looked to innovative solutions. The learning from COVID-19 is already changing the way some low vision services are delivered. We encourage all commissioners and providers of eye health services to review their current low vision assessment service provision, particularly use of remote consultations for pre-assessment review and follow up /monitoring; and their processes for ensuring equitable access to services meeting consistent standards of care. The development of more integrated low vision services has significant benefits for patients, practitioners and organisations across health and social care. The CCEHC will be considering further phases of work to monitor progress.#2
Debbie McGill, Head of Policy and Public Affairs for ABDO said, “We were pleased to be involved in this piece of work and ask that NHSE consider the findings with a view to deliver a national low vision service in England to provide our ageing population with the eye care support they need, close to their homes. Dispensing opticians are well placed in optical practices to provide this care and advice.”