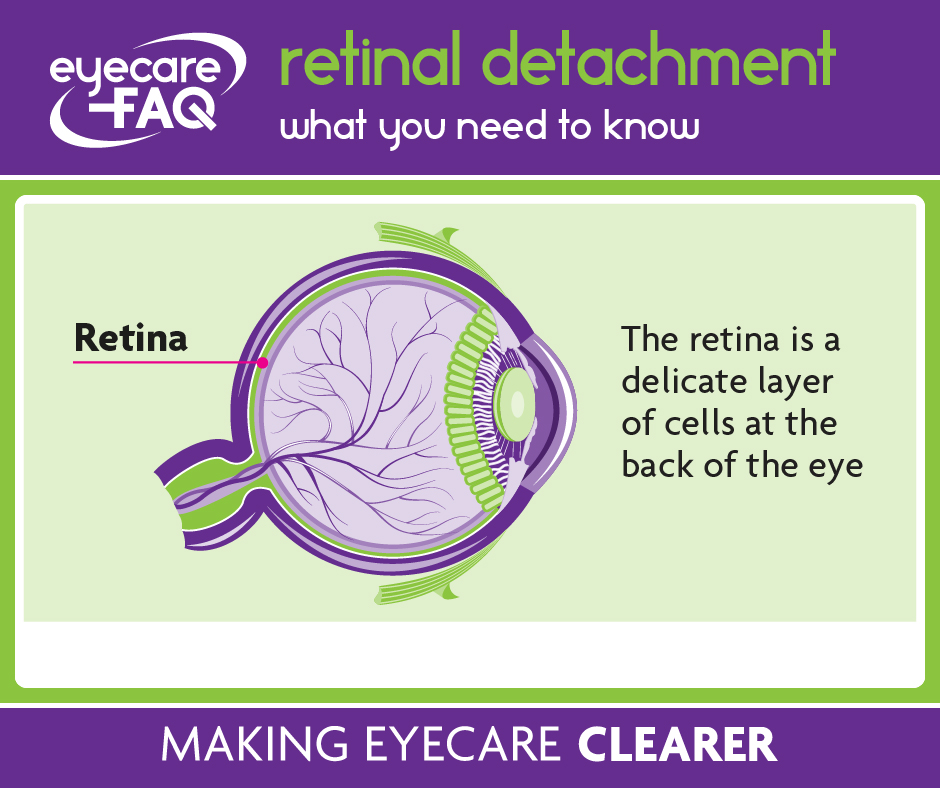
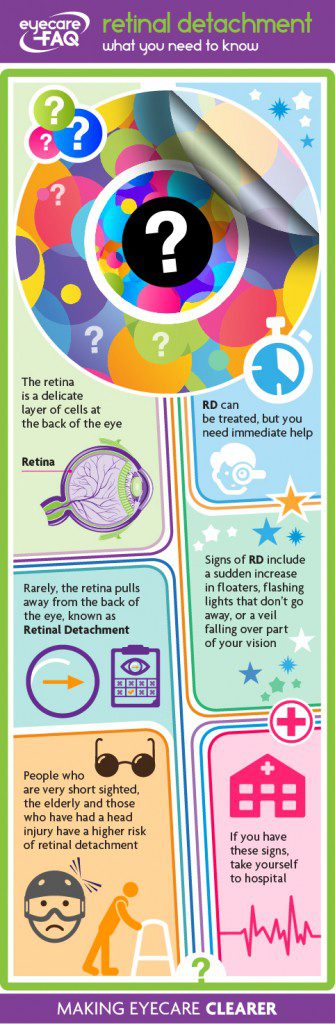
What is Retinal Detachment?
The retina is a delicate layer of cells at the back of the eye. The cells detect light and send signals along nerves to the brain. Very rarely, the retina may pull away from the back of the eye, which is known as retinal detachment. This can be treated, but immediate action is needed to do so. If you have a sudden increase in floaters, flashing lights that don’t go away, or a veil falling over part of your vision seek immediate treatment from accident and emergency.
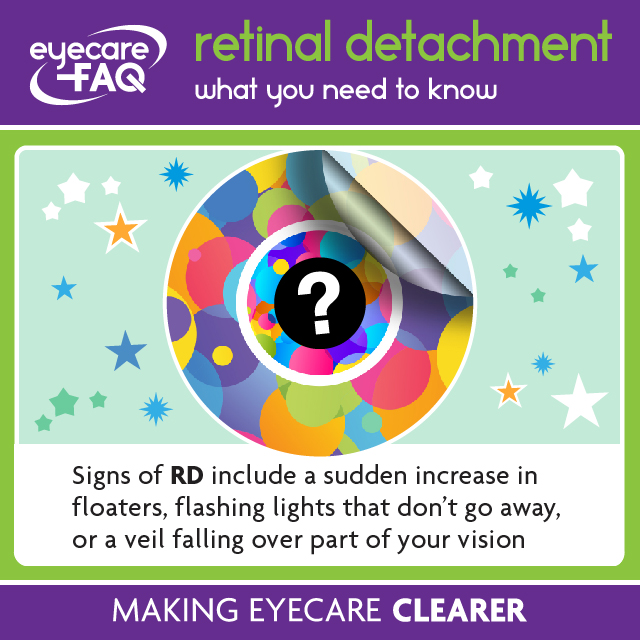
What are the signs of retinal detachment?
If you are experiencing a retinal detachment you may notice a sudden increase in floaters (black or translucent spots or lines) and the start of flashing lights which don’t go away. An area towards the edge of your vision may become blurred. You may notice a shadow or veil fall over part of the edge of your vision. If you have a combination of these signs seek help straight away.
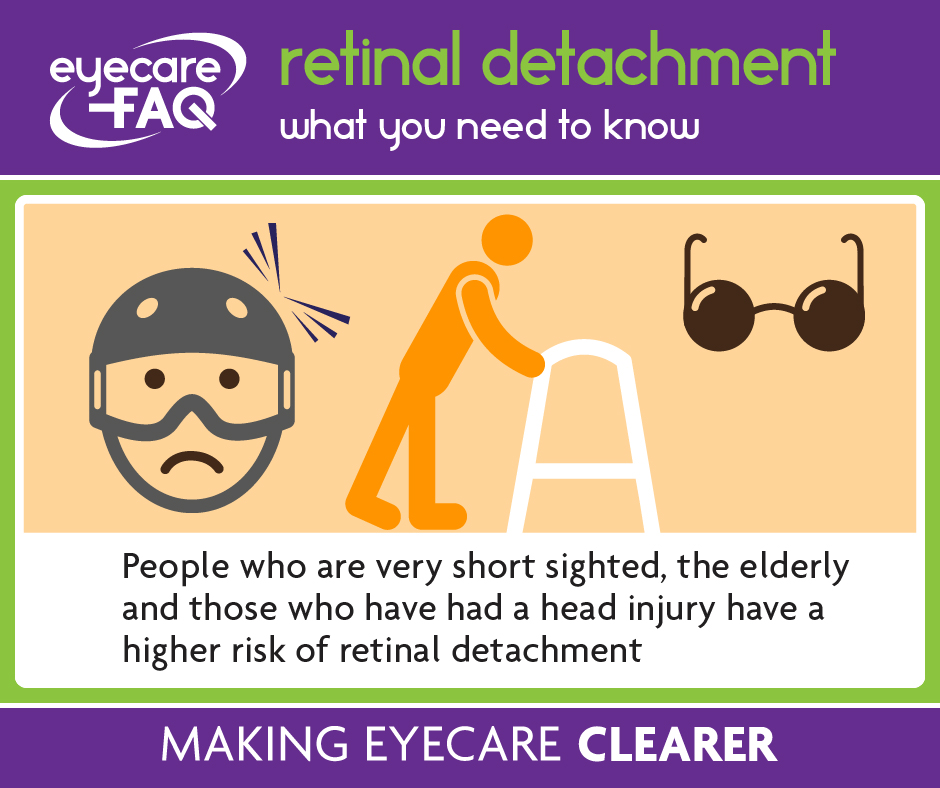
Who is at risk of retinal detachment?
People who are very short sighted have a higher risk of retinal detachment. This applies to you if your spectacle prescription is -6.00 DS or greater. Retinal detachment can happen after a blow to the eye or head, sometimes immediately after the accident, but also in the next few days or weeks. Retinal detachment is more likely to happen in older people. Sometimes it may occur after cataract surgery but this is more likely to happen if you are very short sighted. People with eye disease due to diabetes or sickle cell may have scarring inside the eye which can lead to retinal detachment.
Why does retinal detachment happen?
The retina can peel away gradually if a small tear or hole in the retina lets fluid seep in behind it. Inflammation or injury can also cause fluid to build up under the retina without the presence of a hole. Scar tissue inside the eye, such as that from diabetic eye disease, can contract and pull the retina away from the back of the eye.
I’m worried I might be having a retinal detachment: what should I do?
If you have any signs of retinal detachment – flashes, floaters or a veil over part of your vision – you should go immediately to accident and emergency so that a specialist eye doctor, an ophthalmologist, can check the back of your eye. The doctor will use eye drops to get a good look inside your eye with a bright light. You will find that your vision is blurred after this and you will need someone else to drive you home.
What is the treatment for retinal detachment?
Some small detachments can be treated under local anaesthetic using a laser or freezing, known as cryotherapy. More often, you will be given a general anaesthetic. Oil or gas may be injected into the eye to hold the retina in place until it reattaches. Gas will reabsorb, but oil may then need to be removed in a second operation. A silicone band can be used on the outside of the eyeball to push it in towards the retina to allow it to reattach. This band is permanent.
What do I need to do after treatment for retinal detachment?
Your eye may be swollen and sore for a few days after the operation. You may stay in hospital overnight. Some people may need to keep their head still for some days after certain sorts of treatment. You will need to use eye drops for some weeks after the surgery. Your vision is likely to be blurred after the operation but may improve over the next few weeks. If the central part of the retina detached your vision for small detail may be permanently affected. If you find you are struggling due to decreased vision, ask your doctor for a referral to your local low vision service or call the RNIB helpline.
Why do I have black dots in my vision?
Have you seen small black dots in front of your eyes? Many people have ‘floaters’, which are small irregularities in the gel inside the eye. You might be aware of threads that appear to float in front of your vision, or something that looks like small pieces of cobweb. These spots and threads can be semi-transparent or dark, and are called Floaters. Often you are unaware that you have floaters: if they have been there since birth your eye and brain learn to ignore them. If you move your eye to try to look at a floater it is likely to move away in the direction you move your eye. You might only see them if you are staring at a light coloured surface or at the sky during the day.
Most of the time, floaters are remnants from when the eye developed. If you have this sort of floater you may have been aware of them for many years. For other people, the number of floaters increase with age. Occasionally an increase in floaters can be a sign of problems inside the eye. Some people find floaters a nuisance if they are visible much of the time, but most people become used to them. They rarely cause problems with vision.
Why do Floaters occur?
Floaters are small dots in your vision. Some floaters are present from birth. Others occur as the gel in the eye, the vitreous humour, shrinks over the years. The gel separates into a watery fluid with wavy collagen fibrils which are seen as line-shaped floaters. Sometimes the gel shrinks enough to collapse away from the lining at the back of the eye, the retina. Once the gel has collapsed, some people see a large ring shaped floater. Occasionally some eye diseases that cause inflammation can increase the number of floaters in the eye.
Who is at risk of Floaters?
Floaters are more common in people who are quite short sighted. They may increase if you have had an eye operation, like cataract surgery, or other eye trauma.
What might happen if I have Floaters?
Most of the time floaters are harmless. Sometimes they may be annoying, but treatment is not advised. Occasionally a sudden increase in floaters may be a sign of more serious eye disease. The retina, a light sensitive layer, pulls away from the back of the eye. This is known as a retinal detachment and may lead to a SUDDEN increase in floaters. This needs immediate medical attention. Take yourself to eye casualty / accident and emergency.
I have flashing lights before my eyes – what are they?
Do you see flashes of light in front of your eyes for no obvious reason? This can be small sparkles or something like lightening or fireworks. Flashes occur when there is a pull on the retina, a layer of cells at the back of the eye that it vital for vision. This might happen as the gel inside the eye, the vitreous, becomes more liquid and collapses. You may experience flashes occasionally, off and on over weeks or month. Flashes can also occur if you are hit in the eye.
When are flashing lights before the eyes a problem?
Sometimes flashes of light before the eyes just indicate a pull on the retina and nothing more. However constant or permanent flashes can be a sign that the retina is pulling away from the back of the eye, known as a retinal detachment. A retinal tear or retinal detachment may lead to a SUDDEN increase in floaters as well as flashes. You might notice a shadow at the edge of your vision too. This needs immediate medical attention. Go to your local accident and emergency or eye casualty department at the hospital if you suddenly notice flashes of light. An ophthalmologist will need to use eye drops and a special light to look inside your eyes to check if the retina is damaged.
Are flashing lights before the eyes related to migraine?
Flashing lights in front of the eye can be due to migraine. Some people with migraine experience an aura half an hour or so before the headache and nausea or vomiting starts. The aura can include shimmering or zigzag lines which may block part of your vision. Some people can experience the flashing lights without going on to have a headache. If you have flashing lights for a limited period of time which then pass off entirely these may be related to migraine. Talk to your GP if this is a new experience for you.