Focus on … DED assessment
Assessment
These assessments should be conducted in an order which goes from least invasive to most in order to reduce the effect of one on the other.
The three areas for consideration are8:
- Non-invasive Tear Break Up Time (NITBUT)
- Tear film osmolarity
- Ocular surface staining
1. Non-Invasive Tear Break Up Time
Where possible it is recommended that Tear Break Up Time (TBUT), that period of time between a complete blink and the first observed break in the tear film, is measured in a non-invasive way to reduce the test itself affecting the result.
The traditional method of instilling sodium fluorescein into the tear film to observe the break up is recognised to have an effect on the tear film itself as well as the potential to affect tear production through reflex tearing. It may be assumed that to measure non-invasively requires the use of expensive specialist equipment, and whereas a keratograph or topographer with the necessary functionality to objectively record the NIBUT in great detail is probably the best option, using equipment which is more likely to be present in any practice is just as acceptable as a method of assessing this. For example, using the mires of a one position keratometer or a placido disc.
If there are no non-invasive techniques available in the practice then the use of fluorescein to observe the TBUT is indicated, however care needs to be taken to observe best practice regarding the amount and concentration of stain instilled. An accuracy of timing in order to reduce the challenges of subjectivity on the assessment is also required. This remains by far the most common method of collecting this information in practice. Due to the more invasive nature of using fluorescein, if osmolarity is being measured then this should be done before the instillation of the stain.
The cut off for a positive diagnostic result is 10 seconds or less.
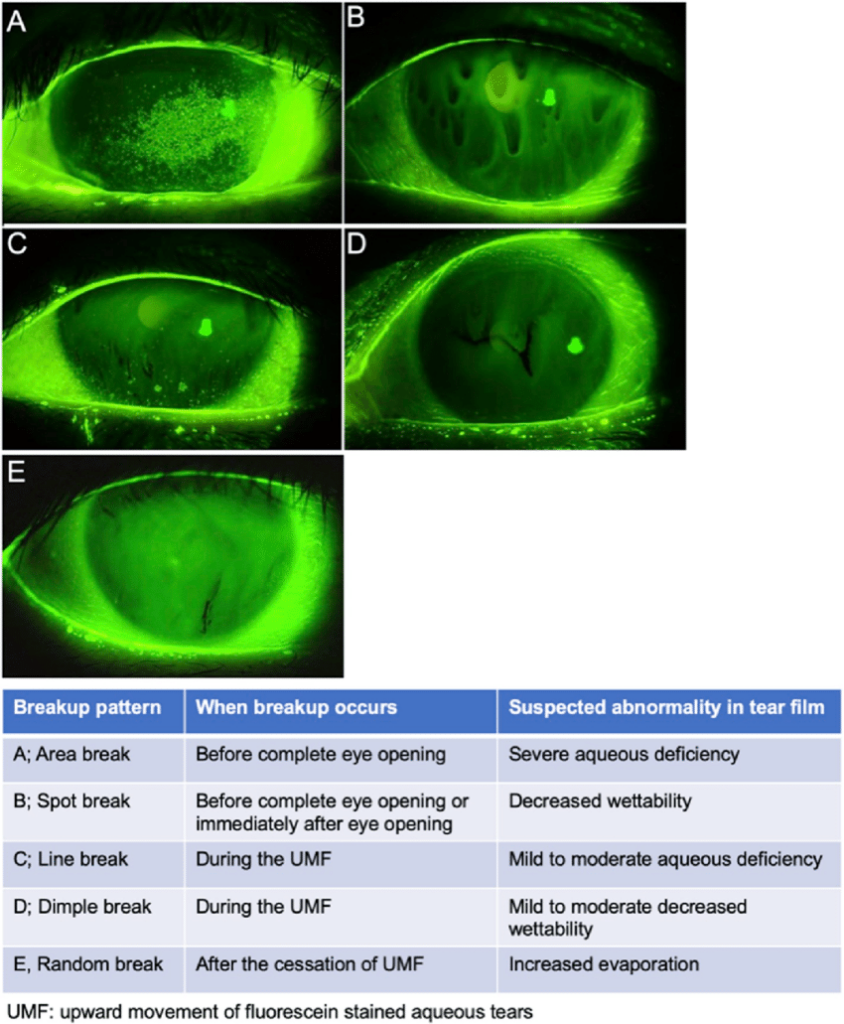
Slit Lamp Images of BUT after instillation of fluorescein
Mires utilized to access TBUT
2. Tear film osmolarity
At this time assessing tear film osmolarity in practice is still relatively rare due to the capital outlay of the specialist equipment required and reported variability of results in subject with high levels of hyperosmolarity as is expected with more severe DED. However, it remains that hyperosmolarity is recognised and the main mechanism of developing DED and evidence of its presence and reduction as a result of management is valuable to both practitioner and patient. Because of this we will only reference the diagnostic cut off values here. A reading of 308mOsm/L or more, or an interocular difference of more than 8mOsm/L, is indicative of DED.
3. Ocular surface staining
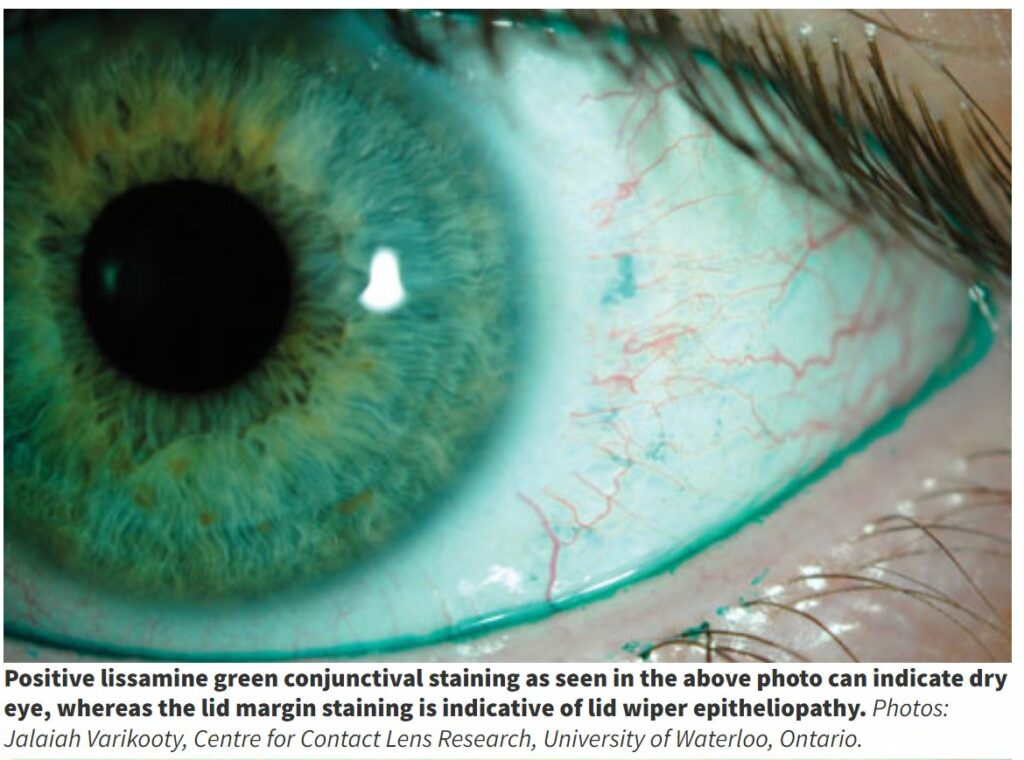
The third area for diagnostic observation is that of ocular surface staining, using fluorescein and lissamine green to observe the cornea, bulbar and palpebral conjunctiva and lid wiper (the contacting surface of the lid which acts to spread the tears across the ocular surface). This is beyond the scope of practice of DOs but is regularly used by CLO/ESCLO and DOs should be aware of the process and results.
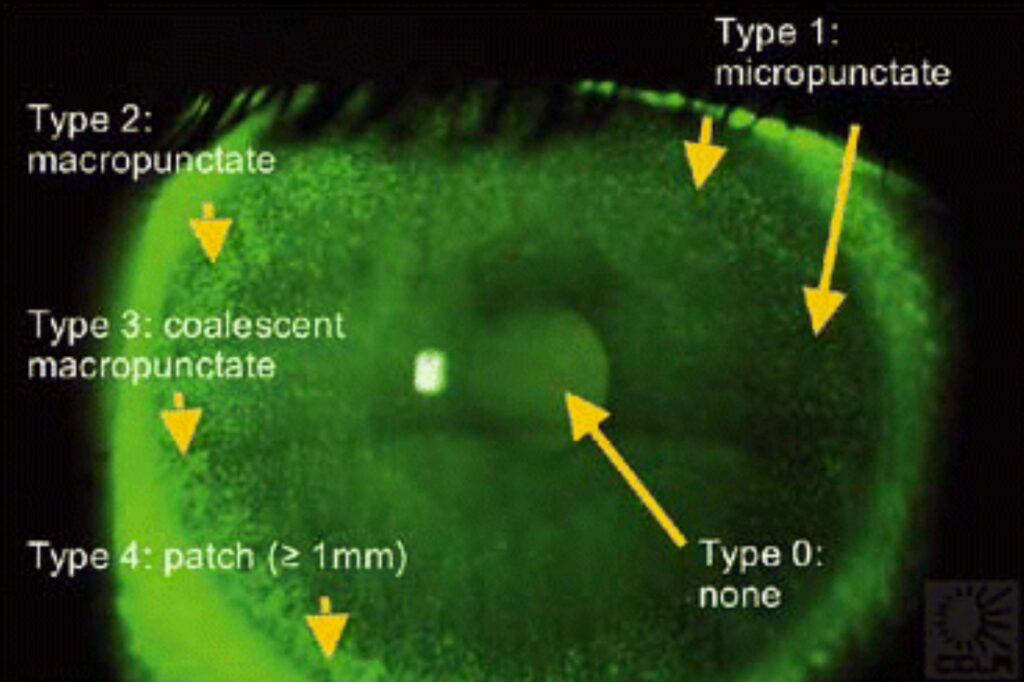
Fluorescein enables a good observation of corneal staining and is best observed on the slit lamp with the cobalt blue light and a yellow (500nm) filter. Conjunctival staining and lid wiper staining is best revealed using lissamine green observed with white light and a red (567-634nm) filter to increase the contrast.
The diagnostic cut offs for these are corneal staining > 5 spots, conjunctival staining >9 spots, and for lid wiper ≥ 2mm of length or ≥ 25 per cent of its width.
Any one of these positive markers being present is taken as an indication of DED.
The presence of any of these three specified signs in either eye, along with positive symptomology, is indicative of a homeostatic imbalance and therefore DED.
If there is a positive result in symptomology and homeostasis markers, DED can be diagnosed and the job of classifying EDE, ADDE, or mixed is possible as well as assessing the severity of DED before deciding a management pathway.
There are many indicators which will point the practitioner to the relevant subtype(s). In normal practice it is recognised that the main indicator for ADDE is the height of the lower tear meniscus being <2mm when measured at the 6 o’clock position. More indicators exist in practice for EDE, mainly being the existence and severity of the various signs of Meibomian Gland Disfunction (MGD). When assessing this the practitioner will consider the meibomian gland (MG) openings, number of blocked or obstructed MGs and the expressability and /or quality of the Meibum. Good meibum should flow easily as a clear oil with gentle pressure, through to a poor meibum being cloudy, thick/buttery and toothpaste like (there is no recognised grading scale for this).
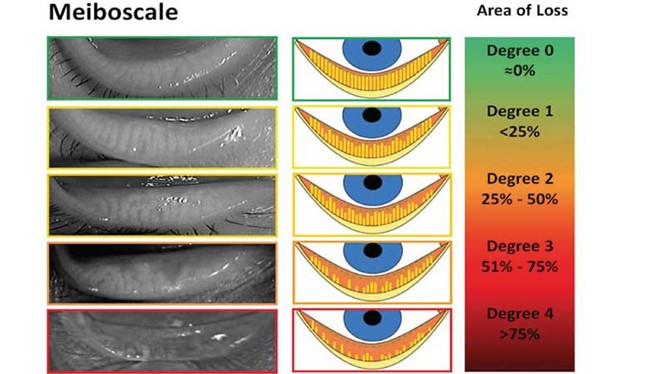
Another way of assessing MGD is meibography, which may be an additional functionality of your keratagraph or topographer, or with the use of a pen-type handheld device, to view the morphology of the MGs in order to grade gland viability, shortening and drop out.